News

Medicare Patients Are Using Fewer Skilled Nursing Services
New research from Avalere finds Medicare beneficiaries are spending fewer days in skilled nursing facilities (SNFs) since 2009 on a per capita basis.

Association Health Plans Projected to Enroll 3.2 Million Individuals
New analysis from Avalere finds that the proposed rule on association health plans (AHPs) is projected to lead to 3.2M enrollees shifting out of the Affordable Care Act's (ACA) individual and small group markets into AHPs by 2022.

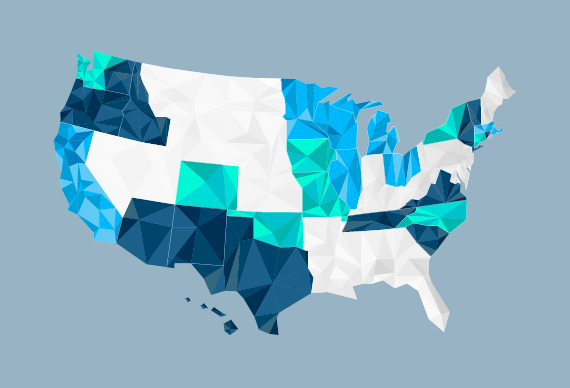
Midwest and Mid-Atlantic States Face Provider Shortage to Address Opioid Epidemic
New research from Avalere Health finds 11 states and DC lack an adequate number of providers certified to prescribe buprenorphine, a medicine used to prevent relapse in people with opioid dependence.

Medicare Part B Payment Increases Will Offset 340B Drug Reimbursement Cuts for 85% of Hospitals
Rural hospitals will see an average 2.7% net increase of Part B payments.

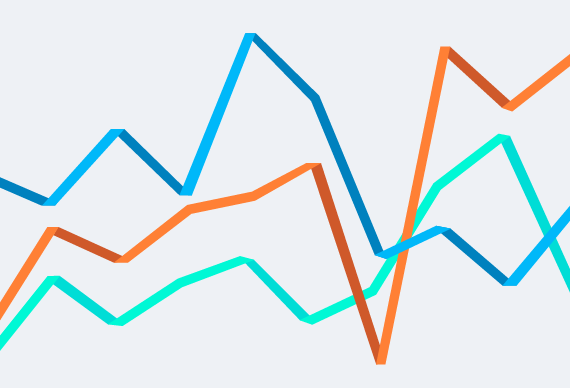
Avalere Analysis Shows that Health Needs and Cost of Medicaid Expansion Populations Grow over Time
Beneficiaries show signs of pent-up demand with acute healthcare needs early in their enrollment, but over time costs increase substantially and shift toward chronic care.

Medicare Financial Incentives Encourage Providers to Take on Greater Financial Risk
While clinicians have been hesitant to assume risk, bonus payments would result in 9 out of 10 ACOs and their participants achieving a net positive financial impact.

Avalere Expands Actuarial and Data Analytics Expertise with Hire of Kenny Kan
Kenny Kan has joined the Avalere team leading the firm's actuarial analytics. Prior to joining Avalere, Kan served as the Chief Actuary at Humana and CareFirst.

Avalere Develops Report on Opioid Analgesic Trends
Resource presents trends in opioid painkiller prescriptions and deaths due to misuse and abuse.

California, North Carolina, and New York Will See the Largest Provider Payment Cuts and Beneficiary Savings Due to 340B Program Changes
Analysis also finds that 62% of impacted facilities will experience less than a 5% reduction in Medicare Part B revenue due to the drug cuts, but 6% of applicable hospitals will experience cuts greater than 10%.
Funding Reinsurance and Cost-Sharing Reductions Would Lower Individual Market Premiums and Increase Enrollment
New analysis by Avalere examines the impact of two market stabilization proposals-funding the cost-sharing reductions (CSRs) and implementing a federal reinsurance program-on individual market premiums and enrollment.

Plans with More Restrictive Networks Comprise 73% of Exchange Market
Deductibles remain high, nearing $4,000 on average for silver plans.

Avalere Welcomes Matt Brow as Executive Vice President and General Manager
Brow was most recently regional SVP of The US Oncology Network for McKesson.
Broader Federal Flexibility for Medicaid Expansion Rules Could Increase Coverage in Both Medicaid and Exchanges
If federal government permits states to expand Medicaid to only 100% of poverty, nearly 4M people could shift from Medicaid to exchanges, and 7M could be newly eligible for coverage.

Most Counties Will Have Free 2018 Exchange Plans for Low-Income Enrollees
New analysis from Avalere finds that nearly 98% of counties with exchanges operated by HealthCare.gov will have free bronze plan options for low-income consumers aged 50 earning 150% of poverty or less ($18,090 for an individual or $36,900 for a family of four).

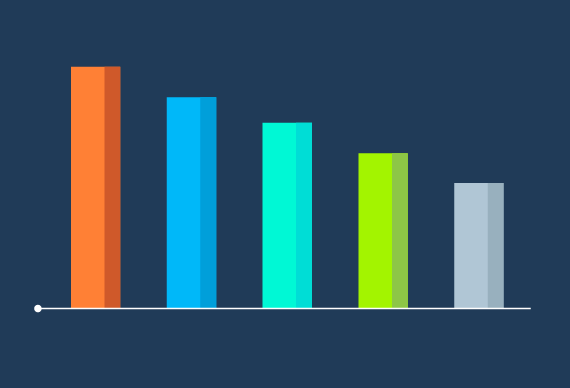
Silver Exchange Premiums Rise 34% on Average in 2018
New analysis from Avalere finds that the 2018 exchange market will see silver premiums rise by an average of 34%. According to Avalere's analysis of filings from Healthcare.gov states, exchange premiums for the most popular type of exchange plan (silver) will be 34% higher, on average, compared to last year.
Uncertainty Reigns as Consumers Begin to Make Health Insurance Decisions for 2018
Avalere experts preview the 2018 ACA open enrollment season
Administration’s Decision to End Cost-Sharing Reduction Payments Will Lead to Substantial 2017 Losses for Health Plans
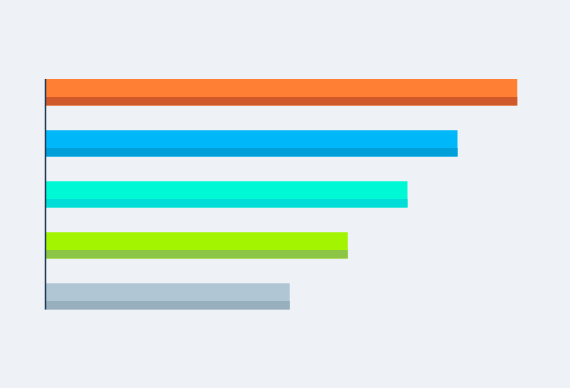
New analysis from Avalere finds that the administration's decision last week to end federal funding for the cost-sharing reduction (CSR) payments could lead to substantial losses for health plans-ranging from -$1.2M in North Dakota to -$200M in Florida through the end of 2017 (Figure 1).
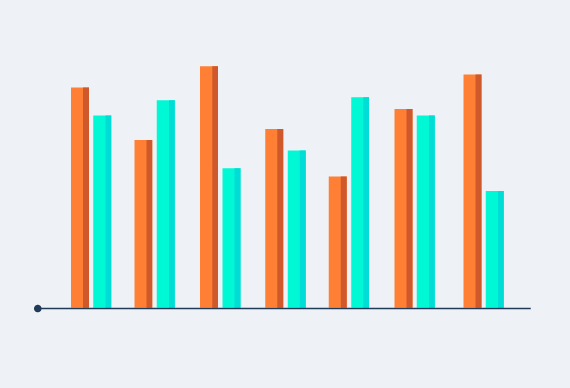
CMS Proposal for New Medicare Payment System Could Lead to Large Payment Variability for Specialists
New analysis from Avalere finds that payments to certain physician specialists could increase or decrease by as much as 16% for their 2018 performance under the Merit-based Incentive Payment System (MIPS).

Beneficiaries in Specialized Diabetes-Focused Medicare Plans Have Fewer Hospitalizations
Compared to beneficiaries with diabetes who are enrolled in other Medicare Advantage plans, enrollees in special needs plans experience better outcomes, after adjusting for demographic and clinical factors.
Updated Analysis: Revised Graham-Cassidy Bill Would Reduce Federal Funding to States by $205B
Avalere has updated its previous analysis to reflect the September 25 version of the Graham-Cassidy-Heller-Johnson (GCHJ) bill to repeal and replace the Affordable Care Act (ACA).




