
Value-Based Care
Alternative payment models are becoming more advanced as the healthcare system transitions to value-based care and payers drive to accelerate generated savings. Track and stay ahead of this evolution to identify strategic partnerships and measure results.

Interview: E3 – The Episode Payment Model and Its Potential Impacts
In the third episode in our bundled payment series, Avalere's Mary Ann Clark discusses how the potential updates may impact device manufacturers.
Interview: E2 – What Mandatory Bundled Payments Mean for Cardiac Care
In episode 2 of our bundled payment series, Avalere's Sally Rodriguez shares how the potential updates may impact post-acute care providers.
New Cardiac Bundles Could Produce Some Big Winners and Losers
Avalere experts say that the impact for most hospitals will be modest.
Interview: E1 – Potential Expansion in Mandatory Bundled Payment Models
For the month of August, Avalere will cover what the new proposed changes to existing bundled payment programs could mean for the healthcare industry. In an exclusive series, experts will discuss what the new bundles include and where to go from here. Kicking off this series is Fred Bentley from our Center for Payment and Delivery Innovation.
Katherine Steinberg, MPP, MBA Joins the Avalere Center for Payment and Delivery Innovation™
Katherine Steinberg comes to Avalere Health with more than 15 years’ experience in the healthcare arena.
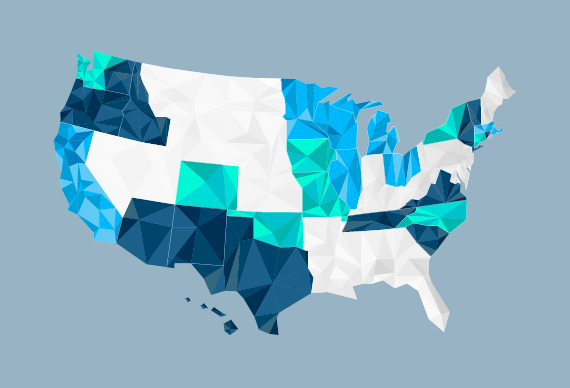
Providers Across the US Express Interest in Moving to New Cancer Payment Model to Control Medicare Costs
Earlier today, the Centers for Medicare and Medicaid Services (CMS) released participation information for its new Oncology Care Model (OCM) slated to begin July 1.
Webinar: Performance-Based Risk-Sharing Arrangements: What Are the Views from the Negotiating Table?
Shifting to a value-based purchasing (VBP) system provides opportunities to engage payer and provider customers in unique contracting and reimbursement relationships that may optimize market access.

Costs of Care: Getting the Patient-Clinician Conversation Right
Avalere Supports the Robert Wood Johnson Foundation in Issuing Two Calls for Proposals
Webinar: MACRA: Preparing for a Revolution in Physician Payments
One year after Congress passed the Medicare Access and CHIP Reauthorization Act (MACRA) in a landslide, the Department of Health and Human Services is implementing this legislation to transform physician payment.
Interview: ACO Prioritization
Avalere's Biruk Bekele talks about a new model Avalere has developed to help life sciences companies more effectively target ACOs and customize their value propositions in the diabetes space based on ACO performance. The number of ACOs has grown rapidly in the past few years, reflecting the Department of Health and Human Services’ push to move 50% of Medicare spending to value-based payment models by 2018.
Interview: Lessons from BPCI and Its Implications for CJR
Our experts share the lessons that we’ve learned from our extensive experience with the Bundled Payments for Care Improvement Initiative. The Bundled Payments for Care Improvement demonstration is a voluntary program sponsored by CMMI in which hospitals, physician group practices, and post-acute care providers accept clinical and financial risk for patients over specified episode time frames post-hospital discharge.

The Evolving Role of the Center for Medicare and Medicaid Innovation in Achieving Value-Based Payment Goals
The passage of the Affordable Care Act established the Center for Medicare and Medicaid Innovation (CMMI) to help advance new payment and delivery models.
Interview: Setting Up a Gainsharing Agreement in CJR
In order to better coordinate care across the care continuum, CMS is allowing hospitals to establish “CJR Collaborators” or other providers that share risk with the participating hospital. Fred Bentley and Erica Breese discuss the details.
Interview: What Is an APM According to CMS?
The Medicare Access and CHIP Reauthorization Act (MACRA) passed last spring is transforming physician payment and standardizing requirements for APMs. Adam Borden and Jared Alves cover Advanced APMs, incentives CMS offers for providers to participate in APM, and the exclusion of specific tracks.
Webinar: CJR and Beyond: Excelling in an Era of Mandatory Bundled Payment Models
With the launch of the Comprehensive Care for Joint Replacement (CJR) model on April 1, CMS has ushered in a new phase for payment reform. Under this mandatory program, roughly 800 hospitals across the U.S. will assume financial accountability for the cost of all services provided to Medicare patients during 90-day care episodes for hip and knee replacements.

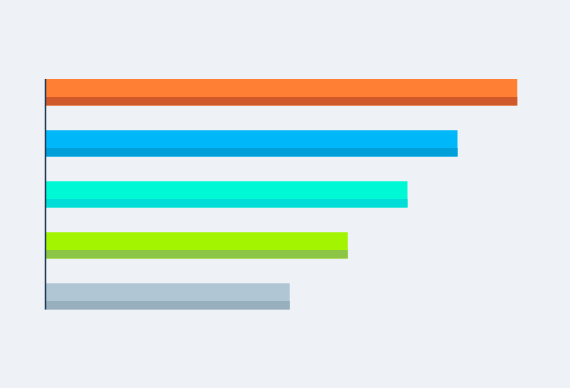
Programs Contributing to HHS Meeting Its Alternative Payment Model Goal Largely Consist of Upside-Only Models
HHS confirms continued movement away from traditional FFS payments, yet significant work remains to move more providers away from upside-risk models and into downside-risk models.

Sixty Percent of Hospitals Must Reduce Care for Joint Replacement (CJR) Costs Under New Medicare Demo or Face Penalties
Hospitals should focus on care after discharge, which drives more than 39 percent of spending.

New Avalere Analysis Finds Profit Margins for Freestanding Skilled Nursing Facilities in Pennsylvania Decreased Almost 30 Percent between 2007 and 2014
According to a new analysis by Avalere, total profit margins for freestanding skilled nursing facilities (SNFs) in Pennsylvania decreased 28 percent between fiscal years (FY) 2007 and 2014, from 3.2 percent to 2.3 percent.
Kindred Partners with Avalere and Inovalon to Support Value-Based Payment in Post-Acute Care
Avalere and Inovalon have entered into a multi-year agreement with Kindred Healthcare, Inc., the nation’s largest provider of post-acute care (PAC) services, to deploy the power of data and analytics to engage payers. The combined solutions will result in a data-driven platform that will support Kindred in improving clinical outcomes and promoting coordinated, efficient care under new value-based payment models.

Participation in Risk-Bearing Accountable Care Organizations Triples; CMS Proposes Rule on Medicare Shared Savings Program Benchmark Methodology
The Centers for Medicare & Medicaid Services (CMS) announced that 121 new Medicare Accountable Care Organizations (ACOs) have joined the Medicare Shared Savings Program (MSSP) and Next Generation (Next Gen) ACO models. In addition, 147 MSSP ACOs renewed their contracts. The increase in risk-bearing ACOs and the recently released proposed benchmark rule mark CMS' commitment to shifting from volume to value.




